Men's mental health in Australia is a critical issue, with a staggering 43 per cent of men between the age of 16-85 reporting a mental disorder at some point over their lifetime. This highlights the importance of skilled mental health professionals who understand the unique pressures men encounter, from societal expectations, cultural differences as well as geographical and emotional isolation.
This article covers how the healthcare workforce can prioritise men’s mental health with advanced knowledge of the distinct factors that impact men. Upskilling in postgraduate mental health study also helps support men with evidence-based, meaningful care that can help promote better mental wellbeing.
Men’s mental health facts
Australian men come from diverse backgrounds, with differences in age, education, culture, language and socio-economic standing, all influencing their mental health. This means that every man’s mental health experience will vary and may present differently to other men. Importantly, biological differences also mean that men’s mental health experiences will also be distinct to women’s.
The National Men’s Mental Health Strategy 2020-2030 reveals that Australian men suffer from a range of mental health conditions across different demographics and life stages. Men’s mental health has such far-reaching impacts that it sits at the top of the list of this government initiative of men’s health issues that need to be addressed.
One of the more alarming men’s mental health statistics shows that suicide is approximately three times more common in men compared to women.
The report also shows that 17 per cent of men aged over 18 self-report poor mental wellbeing, while 23 per cent of males aged between 16-24 experience mental illness symptoms to varying degrees. Moreover, substance use disorders are twice as prevalent in men than in women.
There are also sociodemographic factors that impact mental health among men. For example, Aboriginal and Torres Strait Islander men and men living in rural and remote areas disproportionately experience poor mental health compared to other groups and those in urban areas. Additionally, members of the LGBTQ+ community, men in the criminal justice system, veterans and those with disabilities are also among the highest risk groups for mental health illnesses.
Men’s mental health data across the lifespan
Below is a general snapshot of the mental health experiences among men in Australia throughout their lives.
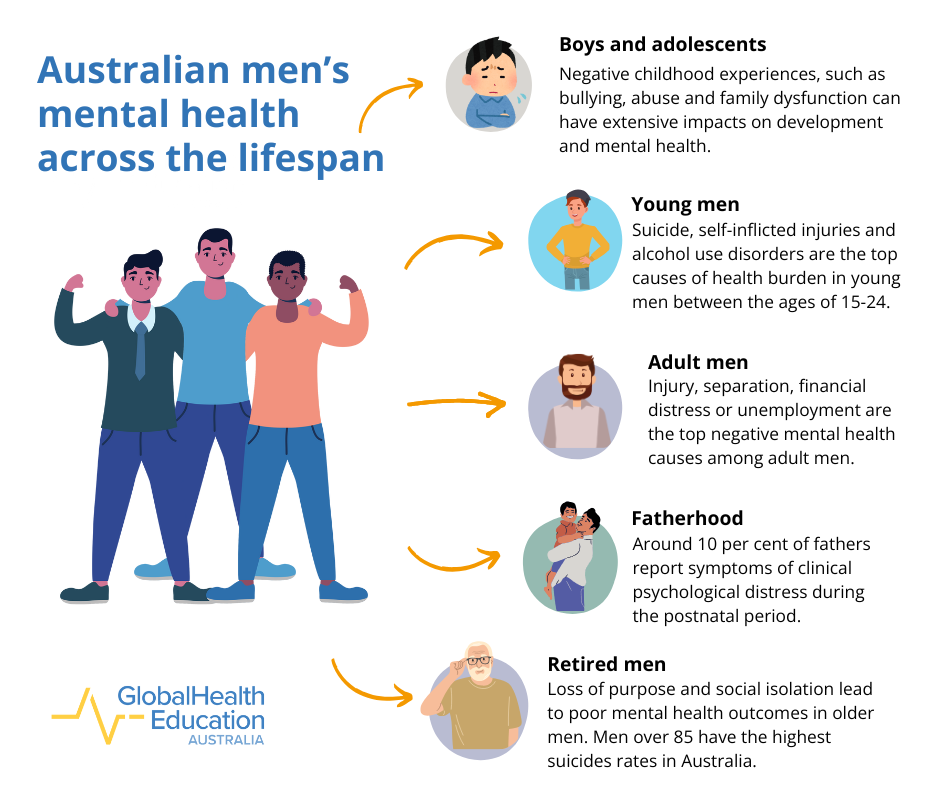
Boys and adolescents
- A healthy lifestyle and positive health system experiences early in a boy’s life are determinants of good healthy habits over the lifespan
- Negative childhood experiences, such as bullying, abuse, family dysfunction or war can have extensive impacts on overall physical and mental health
- Suicide, self-inflicted injuries and alcohol use disorders are the top causes of health burden in young men between the ages of 15-24
- 46 per cent of all suicides in Aboriginal and Torres Strait Islander males occur in those aged between 15-24
Adult men
- Serious illness, injury, separation and divorce, financial distress or unemployment are the top causes of negative physical and mental health outcomes among adult men
- Around 10 per cent of fathers report symptoms of clinical psychological distress during the postnatal period
- Self-inflicted injuries and suicide remain the leading cause of fatal burden among men between the ages of 24 and 44
Older men
- Among older Australian men, major and chronic illness, loss of a partner and financial distress negatively impact mental health
- Further life experiences such as retirement, loss of purpose and social isolation are prevalent issues that lead to poor mental health outcomes among men
- Men over the age of 85 have the highest suicide rates in Australia
A clinical perspective on men’s mental health
Luke Lawrence from Explore Psychology sees male clients across the lifespan. The mental health challenges presented among these clients in his practice are reflective of what the broader data shows above.
He explains that across the younger age range between 16-20, he sees a lot of neurodivergence and issues with anxiety, depression and navigating intimate relationships. Luke also says that younger male clients are interested in developing their social skills and need support with adjusting to adult life, especially with the demands of university study, relationships and work.
As men enter their late twenties, the brain region responsible for executive functioning, which involves planning, working memory and impulse control is more fully developed. Luke says that around “27-28 is when the brain exits the adolescent stage, and we become less impulsive, more in control and more conservative.” Luke adds that from then until around 50, men tend to seek support for various forms of trauma due to a range of life experiences. “People do start to reflect back on the experiences they had, that impacted their development and made them, them,” he says. Luke explains that men in early retirement can also struggle with issues related to anxiety and depression. These can be diagnosed as adjustment disorders.
A strategy to promote men’s positive mental health may be one that addresses needs according to their stage of life. From childhood to retirement, it’s important to recognise that men’s experiences and challenges in various roles and contexts can impact men’s mental health.
Building strong and effective support for men’s mental health
Masculine norms and help-seeking behaviour
In Australia, societal ideals of masculinity that emphasise strength, independence and a ‘she’ll be right, mate’ attitude tend to discourage vulnerability and help-seeking behaviour in men. This emotional stoicism whereby men feel they should be able to handle their issues alone contributes significantly to the stigma around men’s mental health and is one of the biggest barriers that impact men, their families and communities that need them.
Luke believes that the ongoing stigma lies in the way men cope with stress and their attitude towards feelings, as if they are something to suppress or avoid entirely. Emotions like sadness, grief, loneliness and fear are all healthy and are often commensurate with experience. In Luke’s clinical work, he often sees a ‘grin and bear it’ attitude, which is ever present, particularly, among middle-aged men. Finding ways to reduce this stigma in older male age groups is an important step in men’s mental health support.
In younger men, the expectation of self-reliance in regard to mental health is changing. Luke highlights the growing shift among younger men who are proactively seeking support from mental health practitioners. “From what I’ve seen, there is a great deal of engagement in psychotherapy and counselling amongst my younger male client base. They’re generally very aware of their feelings and want to talk about them.”
The value of male-centric mental health services
Health services are not always designed to cater to the unique experiences and needs of men. This lack of gender-specific care extends to men’s mental health services, which include therapeutic environments, specific interventions and delivery modes, which can create another barrier for men seeking support. For instance, if feeling comfortable about discussing their concerns is a primary hurdle, then traditional talk therapy may not always be an ideal approach that men wish to take. Mental health services and resources that cater to men specifically, such as digital or chat-based services, can provide alternatives that differ from face-to-face interactions.
Similarly, ensuring that the mental health workforce has a balance of skilled male and female professionals can help meet the unique needs of men. Women currently make up the majority of professionals in the mental health sector, accounting for 70 to 85 per cent of the workforce. However, Luke says a good proportion of his client base is male. This may indicate that men feel more comfortable seeking support from male practitioners, perhaps because they share similar lived experiences, pressures and challenges. It also shows a likely increased need for men to enter into the mental health sector.
“The vast majority of my clients are men, around 75 per cent. [There’s] definitely seems to be an appeal for most men in seeing a male practitioner.”
Aside from counselling and psychology services that cater to men, there are other initiatives that may be well-suited to meet the needs of men and their mental health. The Australian Men’s Health Forum acknowledges the important fact that men and boys can connect through ‘doing stuff’, rather than sharing emotions. Community programs such as Men’s Shed and Mr Perfect serve as fun opportunities for men to connect with other men over mutual interests and socialising.
For men who enjoy being active, Men’s Walk and Talk Groups and mixed martial arts organisations such as One Roll have provided spaces for men to combine movement and mateship. These men’s mental health organisations can help uniquely and effectively support men and encourage them to seek help when they need it.
Better accessibility in rural and remote areas
There are also clear logistical barriers to seeking support for some men in Australia. Men who live in rural and remote areas face specific challenges, such as accessibility to appropriate mental health resources and professionals. Financial pressures, long working hours and feeling isolated are common experiences for men living and working outside of urban centres. These obstacles could be worse among single or retired men and those with disabilities or belonging to socially disadvantaged groups. Rural and remote areas also tend to have higher suicide, alcohol and substance abuse rates among men, indicating a greater need for appropriate, readily available and effective mental health support.
Telehealth services are integral to these communities, with health professionals offering crucial mental health support to men in rural and remote areas. Men who take advantage of these services can avoid the cost and time output involved with extensive travel which allows them to maintain their ongoing family, work or other responsibilities. Bolstering the rural and remote healthcare sector with mental health telehealth services are important to help address the unique mental health challenges men in these areas experience.
Participating in online peer support groups is another option for men who struggle to find or connect with in-person groups. According to Beyond Blue, engaging in virtual peer-support helps create a healthy, anonymous and judgement-free environment for men to share their concerns. Initiatives like these can help promote help-seeking behaviour, improve outcomes and benefit men with mental health challenges.
Equipping the health workforce to support men’s mental health
Health providers have a unique opportunity to empower men of all ages to take charge of their mental health. Understanding that men’s mental health concerns manifest differently to women’s mental health and that it varies between individual men can help the workforce develop a healthcare approach that adequately meets the needs of male clients.
Postgraduate courses in mental health can help you deepen your understanding of men’s mental health in relation to cultural needs, trauma-informed care, patient-centred care and mental health across the lifespan.
Ultimately, getting to know the man you’re supporting and determining the right approach for him is an important part of delivering high-quality mental health care.
Upskilling with postgraduate mental health courses
If you’re thinking of upskilling with a course in mental health, there are a range of options available to you. Many universities offer general as well as specialised courses for mental health, which can cater to different strengths, interests and career goals.
For postgraduate students, the convenience of online mental health courses offers a flexible delivery mode that fits in with your lifestyle. If you’re a registered nurse looking to specialise in mental health, you have the option to upskill with postgraduate study in mental health nursing.
Whether you already have a healthcare background or are pivoting into the health industry from another field, there are many leading-edge online mental health courses to explore that can help advance your career in the mental health sector.
General mental health courses
Southern Cross University (SCU) Online’s Graduate Certificate in Mental Health, Graduate Diploma of Mental Health and Master of Mental Health courses are tailored for professionals in the health, psychology and social science sectors.
Throughout each course level, you’ll undertake a range of mental health subjects, including Contemporary Mental Health, Mental Health Across the Lifespan, Mental Health in Community, Non-Government and Primary Health Settings and Acute Mental Health.
The SCU Online graduate certificate course equips you with industry-relevant skills in contemporary mental health practices that apply to roles in a range of healthcare settings.
SCU Online’s graduate diploma course is ideal if you want to deepen your understanding beyond the certificate level, with advanced knowledge in evidence-based practices, giving you the confidence to assist patients with different mental health conditions.
Expanding from these is the master’s degree, which is the most comprehensive course geared towards people interested in advanced psychotherapy knowledge and professionals seeking leadership roles in mental health.
The courses below are listed by qualification level, from lowest to highest.






Victoria University (VU) Online’s Graduate Certificate in Mental Health and Master of Mental Health courses are designed for allied health, welfare and social care professionals who want to expand their skills in mental health.
Throughout both courses, you’ll complete different mental health units, including Mental Health Foundations, Recovery-Oriented Mental Health, Biopsychosocial and Cultural Perspectives in Mental Health and Effective Trauma-Informed Care.
In the graduate certificate course, you’ll develop a fundamental understanding of collaborative healthcare approaches in mental health settings. Whether you’re a social worker, physiotherapist, dietitian or optometrist, these skills will help inform your practice, delivering high-quality care rooted in a foundation of mental health.
The master’s degree expands on this knowledge with advanced topics, such as Perspectives of Addictive Behaviours and Mental Health in Later Life. You’ll also gain important skills to lead multidisciplinary mental health teams in different settings.
The courses below are listed by qualification level, from lowest to highest.




ECU Online’s Master of Mental Health is tailored for professionals from diverse backgrounds looking for career advancement in community health, workplace wellbeing and other professional settings. Potential roles available to you following the completion of this course include Mental Health Support Coordinator, Workplace Mental Health Consultant and Mental Health and Welfare Manager.
In this master’s degree, you'll complete a wide spectrum of mental health units, including Acute Mental Health and Crisis Intervention, Community Approaches to Mental Health, Trauma-informed and Recovery-oriented Mental Health Care, and Leadership and Workplace Mental Health. You’ll also undertake an individual work-based research project and choose one elective unit from options including Theories and Techniques in Counselling, Counselling in a Digital World and Mental Health Counselling.
Specialised mental health courses
VU Online’s Graduate Certificate in Child and Adolescent Mental Health and Master of Child and Adolescent Mental Health are unique courses that offer in-demand skills to health professionals in educational and clinical roles in the niche area of child and adolescent mental health.
Throughout both courses, you’ll complete subjects including Mental Health Foundations, Introduction to Child and Adolescent Mental Health, Child and Adolescent Engagement and Assessment, and Effective Trauma-Informed Care.
After completing the graduate certificate, you’ll have a foundational knowledge of mental health, skills required to provide effective mental health interventions and collaborative skills for interdisciplinary healthcare roles.
The master’s degree is a comprehensive course for educators, allied health professionals and those in social care. This course builds on the nested graduate certificate with additional subjects such as Child and Adolescent Mental Health and Wellbeing in Schools, Assessment in Mental Health, Psychological Therapies, Perspectives on Addictive Behaviours and a final Research Project. After completing this course, you’ll be equipped to work with and support the mental health of children and teenagers in various clinical, educational, therapeutic and community settings.
The courses below are listed by qualification level, from lowest to highest.




Strengthen your mental health expertise today
Supporting men's mental health requires skilled and dedicated healthcare professionals who understand the unique challenges men face and what they need to get back on track. Postgraduate study in mental health offers a pathway for you to deepen your expertise, allowing you to deliver targeted support that promotes optimal outcomes for men across diverse ages and experiences.
GlobalHealth Education’s university partners offer healthcare courses in a range of other fields, including social work, public health, counselling, nursing, psychology, leadership and mental health. To take the next step in advancing your healthcare career, browse the course catalogue, choose a course and enquire to speak to a Student Enrolment Advisor for guidance with your enrolment.
For personalised advice, book a professional development strategy call with our Education Consultant today and unlock your potential to make a meaningful difference in men’s mental health.
Men’s mental health resources
Counselling and mental health services
- Beyond Blue
- Black Dog Institute
- Health Direct
- Lifeline
- Mensline Australia
- Rural and Remote Mental Health
- SANE Australia
Resources
Parenting support
Trauma-informed care mental health service
Digital mental health services
Aboriginal and Torres Strait Islander crisis support